The offer letter arrives quietly, a PDF with a salary figure and a tentative start date. For many physicians, it feels final. In reality, it begins a longer process. Doctor relocation often unfolds unevenly, with longer gaps than anticipated between offer acceptance and clinical start. Physicians relocate for fellowships, leadership opportunities, and family needs. Across specialties, relocation has become common.
Each move carries professional, financial, and personal consequences beyond the contract.
Knowing the relocation process helps physicians reduce stress, avoid income gaps, and manage administrative delays.
Stage One – Offer Letter Review and Conditional Acceptance
Relocation starts with the offer letter; however, its significance often goes unnoticed. Meanwhile, while compensation draws attention, relocation terms usually appear later and feel secondary.
At this stage, several relocation-related questions matter –
- Who pays for the move, and how reimbursement works
- If temporary housing is included
- What happens if credentialing delays the start date
- How relocation benefits interact with tax obligations
Physicians who accept offers without clarifying these details often absorb costs later. Relocation stipends may be capped. Reimbursements may arrive months after expenses are incurred. In some cases, benefits disappear if employment ends within a defined period.
A careful review at this stage sets expectations for the remainder of the relocation journey.
Related – Top Cities for Female Physicians to Practice in the United States
Stage Two – Contract Finalization and Start Date Reality Check
Once negotiations conclude and the contract is signed, many physicians mentally commit to the stated start date. That date, however, remains aspirational until several parallel processes align.
Relocation depends on forces outside a physician’s control. In practice, approval bodies follow set timelines. Early start dates prove unrealistic.
Experienced relocation advisors often recommend building flexibility into the contract itself. Language that ties the start date to completed credentialing protects both physician and employer from frustration.
At this stage, clarity matters. In particular, understanding how delays affect compensation is critical. Confirm relocation benefits and onboarding expectations early. Contract finalization allows flexibility when timelines shift.
Stage Three – State Licensing and Medical Board Approval
Licensing represents the longest and least predictable segment of relocation. Physicians moving across state lines encounter different requirements, processing speeds, and documentation standards.
Some states issue licenses within weeks. Others take several months. Missing transcripts, delayed verifications, or background check discrepancies can reset timelines entirely.
As licensing progresses, income frequently pauses. Without approval, clinical work remains on hold while expenses increase.
Understanding that relocation includes this financial exposure allows physicians to plan reserves or negotiate bridge support when possible.
Stage Four – Credentialing and Privileging at the Hospital Level
Licensing alone does not authorize practice within a hospital. Credentialing and privileging follow, and these steps operate independently from state boards.
Hospital committees verify credentials and references. However, they meet on fixed schedules. Missed deadlines cause weeks of delay.
Relocation timelines often stall here, not because of physician error, but because institutional processes move slowly by design. Hospitals prioritize risk mitigation over speed.
Physicians often assume approval is close until delays become apparent. Clear communication during this stage reduces uncertainty and prevents premature moves.
Stage Five – Insurance Enrollment and Payer Alignment
Even after credentialing approval, relocation remains incomplete until insurance and payer enrollment align. In practice, delays here can leave physicians on-site without billing access.
This phase directly affects revenue, compensation structures, and workload distribution. In productivity-based roles, delayed enrollment can reduce earnings while moving expenses continue. Employers provide interim income coverage or travel insurance during this window. In others, physicians must absorb the risk.
For physicians relocating into private practices or hybrid roles, financial exposure tends to increase. Therefore, understanding health insurance timelines helps set realistic expectations. In addition, clear insight into payer enrollment supports securing appropriate protections. Relocation costs remain controlled before they escalate.
Also read – Top 10 Digital Nomad Insurance Providers: Protecting Your Global Adventures
Stage Six – Housing, Family Logistics, and Physical Move
While administrative processes unfold, physicians still must relocate physically. In many cases, housing decisions happen before timelines settle. Short-term rentals or extended stays become common.
Relocation rarely affects physicians alone. Meanwhile, spouses change jobs. At the same time, children change schools. In turn, support systems reset. All of this occurs while professional uncertainty remains unresolved.
Physician burnout research repeatedly links relocation stress to higher strain. This effect grows when moves coincide with demanding workloads or leadership transitions. Integrating housing and family planning into relocation lowers lasting stress.
Stage Seven – Pre-Onboarding and Institutional Orientation
Hospitals initiate onboarding. At this stage, activities include electronic health record training, compliance modules, policy reviews, and departmental orientation.
At first glance, onboarding may appear procedural. However, it shapes early professional relationships. Physicians who arrive exhausted from prolonged relocation stress often struggle to engage fully during this phase.
In turn, compressed onboarding during early clinical weeks raises dissatisfaction. Physicians struggle to adjust to new systems and expectations. By contrast, onboarding that occurs before clinical duties begin creates space for adjustment.
Consequently, physicians report smoother transitions and stronger integration.
Stage Eight – First Day on the Floor
The first shift carries symbolic weight after months of paperwork, uncertainty, and logistics; clinical work resumes. However, relocation effects continue long after this moment.
Meanwhile, physicians may still lack local networks. Commutes feel unfamiliar. In addition, systems differ subtly from prior roles. Over time, productivity stabilizes gradually.
In practice, hospitals that treat relocation as complete on day one often miss opportunities to support retention. By contrast, those that extend relocation support into the first six months see stronger engagement and lower turnover.
At this stage, sustained support matters. Regular check-ins and clear expectations help physicians settle more quickly. Continued support improves integration.
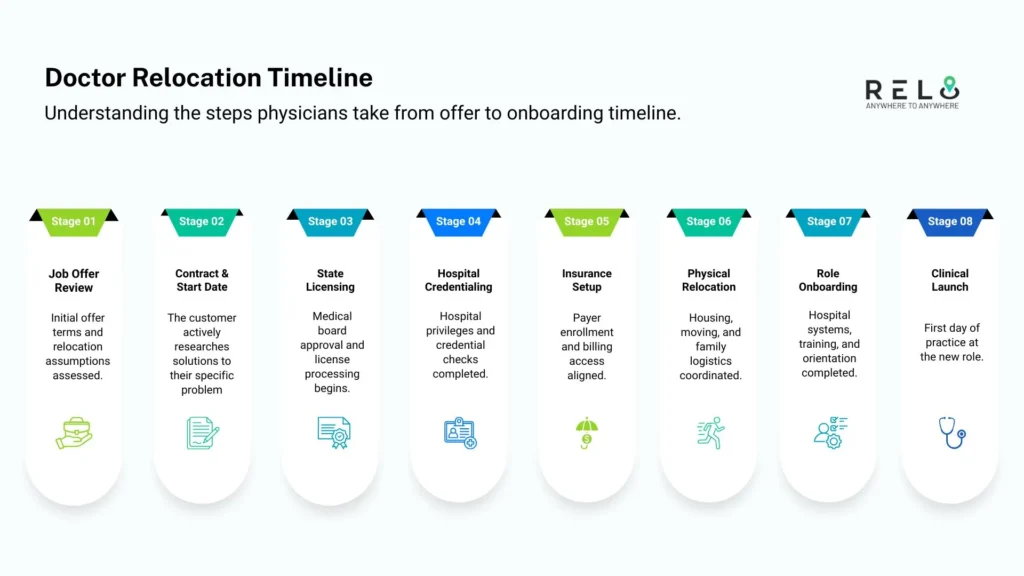
Doctor Relocation Timeline From Offer to Clinical Start (PDF)
Relocating for a medical role involves far more than accepting a job offer. In practice, this relocation timeline maps each key phase, from offer review through licensing, credentialing, housing, and hospital onboarding.
Along the way, the timeline clarifies next steps, helping physicians plan around delays, costs, and start dates. Each stage reflects real administrative milestones.
Designed for physicians changing hospitals, systems, or states, this timeline keeps decisions structured and expectations aligned.
Download Now (High-Quality PDF Version)
Recommended read – Your 30-Day Relocation Calendar with Daily Actionable Steps
Why the Doctor Relocation Timeline Deserves Attention
Relocation often shapes physician satisfaction. Without structure, even strong roles can lose appeal. With proper support, trust forms before clinical pressures rise.
Evidence from physician staffing firms shows early departures often link to relocation friction. Delays, unplanned costs, and family disruption quietly erode commitment.
As a result, physicians who understand the relocation timeline negotiate clearly, plan ahead, and prepare for delays others overlook.
How to Speed Up Doctor Relocation Without Creating Risk
Speed in relocation comes from preparation, not pressure. Physicians who move efficiently focus on coordination rather than rushing steps that carry regulatory or financial consequences.
The following actions consistently shorten relocation timelines without increasing exposure –
- Prepare documents early – Collect licensing forms and verifications upfront.
- Run steps in parallel – Move licensing, credentialing, and housing together.
- Centralize coordination – Assign one point of oversight.
- Set realistic start dates – Match start dates to approval timelines.
Relocation accelerates when systems are aligned, and expectations are clear. Precision and planning move physicians faster than urgency ever does.
In addition, speed improves with visibility. Tracking approvals and adjusting assumptions early prevents last-minute disruption. Relocation moves fastest when progress is monitored deliberately.
A Complete Doctor Relocation Support That Reduces Risk
A medical relocation extends beyond a change of address. Licensing timelines, credentialing steps, housing decisions, and start dates shape the transition.
Relo.AI supports relocation through coordinated planning and data-driven guidance. By addressing timing risks, financial exposure, and administrative requirements early, physicians avoid rushed decisions. From offer review to hospital onboarding, each step remains aligned.
To further support planning, we provide a relocation cost estimator that offers early visibility into expected expenses and financial gaps. Clear data replaces guesswork, keeping relocation decisions deliberate.
For complete doctor relocation support, visit HERE for more details.
Bottom Line
Doctor relocation extends far beyond accepting an offer letter. Licensing, credentialing, housing, and onboarding shape the transition long before the first shift begins. Physicians who understand the full relocation process plan more effectively and avoid unnecessary disruption. Employers who acknowledge this complexity improve retention and reduce early friction.
Careful management of every step determines whether relocation succeeds long before day one.
Doctor Relocation Support Across Every Stage of the Transition
Relo.AI guides physicians through relocation with coordinated planning from offer to onboarding.
We support licensing timelines, credentialing workflows, housing planning, and start-date alignment. Coordination with hospital and HR teams prevents avoidable disruption.
Also, we address financial exposure, timing gaps, and compliance early, allowing physicians to relocate with confidence.
Clear data, realistic timelines, and coordinated execution shape every recommendation we provide.
Set up a FREE consultation to structure your relocation process.